Gingivitis is a common but mild form of gum disease, the first sign of which is often bleeding gums. Left untreated, it can progress to a more serious condition called periodontitis – this may result in loss of teeth and the bone supporting them.
Alarmingly, data from the WHO (World Health Organisation) shows more than 3/4 of people aged between 35 and 45 and more than half of adolescents over the age of 15 are affected by some kind of gingival problem.
Gingivitis develops when dental plaque (a film of bacteria on the teeth) isn’t cleaned away properly. Fortunately, if caught in the early stages, gingivitis cures are very effective. Good oral hygiene will help stop it from recurring.
In this article you can read all about the different types of gum disease, what the symptoms are, and the best ways to keep your mouth and gums healthy.
In This Article
What is gingivitis?
Gingivitis is a type of gum disease. Those who have gingivitis may notice swelling or inflammation, as well as tenderness and bleeding, particularly when you brush.
For a brief overview of the condition you can view this short video:
There are three main stages of periodontal (gum) disease. Each displays different symptoms and requires a different type of treatment.
Gingivitis is the most mild form, where the gums are inflamed rather than infected. Catching it at this stage will help prevent irreversible oral damage.
The table below summarises the different phases of gum disease. Keep reading to find out more about causes, symptoms, treatment and prevention.
Gingivitis | Periodontitis | Advanced Periodontitis | |
Symptoms | Red, swollen or bleeding gums; bad breath | Tartar (calculus) build-up; receding gums; loose teeth | Loose teeth; pain while eating |
Severity | Mild inflammation of gum tissue | Infection of gum tissue | Severe infection of tissue and bone |
Effects on oral health | No long-term effects if treated early | Irreversible damage to bone and tissue | Destruction of bone and tissue; possible tooth loss or misalignment |
Treatment | Scale and polish with a hygienist; better oral hygiene | Scaling, root planing or dental surgery to remove infection | Dental surgery, possibly bone grafts and tooth extraction |
Prevention | Good oral care and regular dental checkups | Maintain good oral hygiene and check for gingivitis symptoms regularly | Visit a dentist if you think you may have periodontal disease |
What causes gum disease?
Bacteria are constantly present in our mouths from saliva. They feed on particles left in our mouths after we eat or drink and can cause damage to our teeth and gums. These bacteria form a sticky, colourless film on our teeth and gums called dental plaque. Have you ever tried to clean ‘furry’ teeth with a fingernail? The substance you scraped off was plaque.

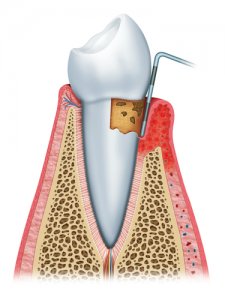
If you don’t clean your teeth properly, bacteria get into the space between the teeth and gums causing inflammation and swelling. Pockets sometimes form in the gums, allowing food to lodge and more plaque to build up.
Plaque hardens over time, forming a hard yellowish-white residue called ‘tartar’ or ‘calculus’. This hard calcareous layer acts as a further breeding ground for bacteria to attack gum tissue.
As periodontal disease becomes more advanced, teeth may become loose and eventually fall out.
A 2018 study from the Oral Health Foundation linked alcohol consumption to tooth decay and gum disease, noting that people who drink every day have higher levels of harmful bacteria in their mouths. Alcohol also affects pathogens that help fight gum inflammation. It’s particularly bad news for wine drinkers, since they produce more of the bacteria that leads to gum disease. Regular beer drinkers, meanwhile, are at greater risk of tooth decay.
Risk factors
Although plaque is the main culprit, certain people are more susceptible to gum disease than others. Those particularly at risk include:
- Teenage girls and menopausal women: Hormonal changes make gums more sensitive and prone to disease. This can affect all women as they go through their monthly menstrual cycle, but hormones are particularly active during puberty and menopause.
- Postmenopausal women: A painful condition called desquamative gingivitis can affect postmenopausal women. The outer layer of the gum detaches from the teeth, leaving them loose and crooked. Nerve endings can then be exposed and cause extreme pain.
- Pregnant women: A nine-month dose of hormones during pregnancy means many expectant mothers notice teeth sensitivity and their gums bleeding. In addition, hormonal variations may lead to localised hypertrophic gingivitis (also known as pregnancy gingivitis). This can be identified by a bright red (benign) pseudo-tumor at the base of one or more teeth that can bleed profusely.
- People with diabetes: Studies have shown a vicious cycle here, with diabetes making periodontal disease worse, and vice versa.
- Smokers: Smoking is responsible for as many as 50% of gum disease cases, as well as many other oral problems, mainly because it increases plaque levels.
- People with vitamin deficiencies: Specifically vitamin C and vitamin B3 (niacin).
- People under severe stress: Acute necrotising ulcerative gingivitis (ANUG) is identifiable by acutely painful, bleeding gums. It often occurs suddenly and as a result of severe stress or a significant traumatic event.
There are other factors which may contribute to gum problems, including:

- Tooth fillings
- Poorly-fitting dental restorations including crowns and bridges
- Crooked teeth (which are harder to clean properly)
- Poor oral hygiene while wearing braces
- Certain medications, including birth control pills
If you are in any of these high-risk groups, particularly if you’re pregnant or going through menopause, be sure to get regular dental checkups so your dentist can deal with any problems quickly.
Recent research from the Oral Health Foundation suggests a link between gum disease and early labour as well. The study found that 45% of women who went into premature labour had gum disease, compared to 29% of women who had a perfect pregnancy.
Is gingivitis contagious?
It is generally understood that most people affected by gum disease have an underlying medical disease or are experiencing hormonal changes that make them more susceptible to bacteria.
But at the same time, these oral bacteria are spread through saliva. Technically, then, gingivitis can be spread by kissing or by sharing utensils and dental equipment. However, if you have healthy gums and maintain good oral health, you shouldn’t be at risk of developing any kind of periodontal disease from contact with someone else.
Gingivitis symptoms
Mild gingivitis is most commonly manifested by the following symptoms:
- Red, swollen gums
- Purple-red patches at the gum line
- Gums bleeding (especially during brushing, flossing or eating)
- Constant bad breath
- A bad taste in the mouth
- Teeth sensitive to hot and cold
Periodontal disease is generally completely painless up to a fairly advanced stage – unlike most dental problems. This, coupled with the fact that there may be no visible symptoms, can make it difficult to diagnose.

Because you probably won’t experience any pain as a warning sign of gum problems, it’s important to be familiar with and regularly check for the symptoms. Otherwise it could develop to advanced periodontitis before you realise something is wrong.
In the later stages of periodontal disease, or with specific types of gingivitis, other more worrying symptoms may develop. These include:
- Loose teeth
- Receding gums
- Teeth shifting position (you may notice they feel different when you bite down)
- Pus oozing from the space between teeth and gums (an indication of tooth infection or abscess)
- Bright red gums
- Dozens of grey or yellow sores appearing on the gums or insides of cheeks
What to do if you have painful or bleeding gums
Don’t be tempted to assume that your gums are bleeding because you brushed a little too hard. Easing off on your brushing may solve the bleeding, but it will just aggravate the underlying cause of gingivitis if that is what you have. A better solution would be to buy a special gum care toothbrush that has super soft bristles to avoid irritating the gums any further.
Read our best electric toothbrush guide or our article on electric toothbrushes for sensitive teeth to find one that will help get your gums in better shape.
It’s better to be safe than sorry, so if you have bleeding or painful gums, or any other symptoms of gum disease, don’t hesitate to see your dentist. The earlier they remove the source of the inflammation or infection, the less chance of it causing lasting damage.
Your dentist will use a small measuring device to check whether your gums have started to separate from your teeth. They will also look for any other indications as to the extent of the problem. If the infection has progressed, they may take x-rays to check for bone deterioration.
How to prevent periodontal disease

The key to preventing gum disease is simply maintaining good oral hygiene. This involves:
- Brushing teeth twice a day for at least two minutes using a fluoride toothpaste
- Flossing at least once a day
- Rinsing with antibacterial fluoride mouthwash
- Using a dental jet to clean hard-to-reach places (especially if you are prone to gingivitis)
- Changing your toothbrush regularly
- Being extra careful with cleaning if you wear braces
- Not smoking
- Visiting your dentist and hygienist regularly, as advised
If you’re unsure how to brush your teeth or floss properly, don’t be embarrassed about asking your dentist or hygienist to show you. Dental professionals want to help you keep your teeth in the best condition possible, so it’s better to ask for help than to just assume you’re doing it right.
The video below explains more about how the correct brushing technique helps keep your gums healthy and prevent decay:
You can also ask your dentist about the best type of toothbrush and toothpaste to use for your teeth.
How to treat gingivitis
If you are already displaying some gingivitis symptoms or are worried you may have an oral infection, speak to your dentist. Although improved dental hygiene can be enough to reverse gingivitis in its early stages, it’s best to get a professional opinion.
Your dentist may just give your teeth a good clean and send you away with some advice for better dental care. They may also provide you with special mouthwash or cleaning tools to prevent future bacterial growth.
It’s more likely, however, that they will conduct a tooth scaling. This is a thorough cleaning and removal of plaque and tartar from above and below the gum line. This treatment may be repeated every three to six months if you are particularly susceptible to plaque build-up.
If you have developed periodontitis your dentist may need to perform a procedure called root planing during a deep teeth cleaning. This involves smoothing out the rough spots on the tooth root so there is less of a surface for plaque to cling to in future.
In advanced cases of gum disease, flap surgery may be necessary. A specialist called a periodontist makes an incision in the gums to access the infected parts of the gum. The infected area is thoroughly cleaned, then the flaps are stitched up so the gums can heal.
The most chronic cases may require a bone graft to restore damaged bone. This is particularly important if a patient plans to have dental implants to replace lost teeth.
Don’t be put off by thinking you might have to have surgery though; these procedures can be avoided by following a good oral hygiene program and seeking treatment as soon as symptoms appear.
Scaling and root planing are dental services intended to provide a healthy tissue environment that will allow tissues to re-adapt to normal tooth surfaces. Periodontal disease, also known as gum disease, is caused by a buildup of plaque, calculus, and stains on the crowns and root surfaces of the teeth. While it can begin as localised gum inflammation, it can quickly progress to serious disease that can cause major damage to the soft tissue and bone supporting the teeth. Scaling and root planing can help treat the disease before it causes the tooth to fall out or have to be extracted.
Dr. Ashley Niles, Niles Family Dentistry
Gingivitis treatment at home
You may be able to combat mild gum problems at home by just improving your dental health routine as discussed above. However, without visiting a dentist you can’t be sure how far the infection has spread.

If you have tartar build-up below the gum line, for example, bacteria will continue to eat away at your gum tissue and bone. No amount of careful brushing can fix this, so it’s best to get a checkup with a professional if you think you may have gingivitis.
Tartar can only be removed with dental scaling. If you can see a white deposit at the base of your teeth, don’t try to remove it at home. Instead, visit a hygienist for professional scaling.
Is treatment covered by the NHS?
The good news is that treatments for gingivitis and gum disease are covered by the NHS.
A basic consultation – including diagnosis, advice, and a scale and polish if necessary – costs £23.80. Any other treatment relating to periodontitis comes under the band 2 treatment charge of £65.20. These prices are correct for 2020/21 in England – read more about NHS dental charges here.
Conclusion
The best way to avoid gum disease is to maintain good oral hygiene and visit your dentist regularly for preventative treatment. Take particular care if you fall into one of the higher-risk groups.
If you notice any symptoms such as swollen, sore or bleeding gums, bad breath, or tooth sensitivity then don’t delay in seeking treatment. It’s far easier to treat an infection in the early stages than once it develops into a more serious condition. Fortunately, it’s only the most severe cases which result in tooth extraction.
World Health Organization (WHO) http://www.who.int/oral_health/disease_burden/global/en/
Consulted 24th April 2019.
National Center for Biotechnology Information https://www.ncbi.nlm.nih.gov/books/NBK279593/
Consulted 24th April 2019.
British Society of Periodontology https://www.bsperio.org.uk/patients/periodiseaseandtreatment.html
Consulted 24th April 2019.
NHS (National Health Service) https://www.nhs.uk/conditions/gum-disease/treatment/
Consulted 24th April 2019.
American Academy of Periodontology https://www.perio.org/consumer/types-gum-disease.html
Consulted 24th April 2019.




