Having pulpitis, or inflamed dental pulp tissue can make your teeth very painful. Fortunately, it’s not too difficult to treat and reverse pulpitis, especially if it’s caught early. If you have been diagnosed with pulpitis or you’re worried you might have it, this guide will help you understand more about this oral health condition.
Perhaps you’re confused about the different terms you’ve heard? Like chronic and acute pulpitis. And what is the difference between irreversible pulpitis and reversible pulpitis?
In this article we’re going to explain:
- The different types of pulpitis
- What causes it
- How it’s diagnosed
- Pulpitis treatment options
Pulpitis is just one of the problems that can cause dental tooth pain. If your teeth hurt, whatever you think the cause may be, we recommend you go for a dental checkup before it gets any worse. But for now, here’s all you need to know about pulpitis pain and treatment.
In This Article
What is pulpitis of the tooth?
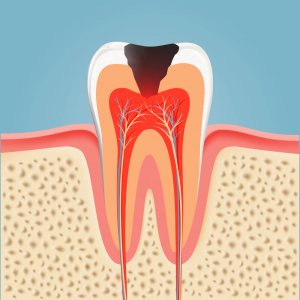
Pulpitis is caused by the pulp in your teeth becoming infected or inflamed. Your teeth have three layers:
- Enamel – the hard outer coating that protects your teeth
- Dentin – the middle layer which supports the enamel
- Dental pulp – the innermost layer with the tooth’s nerves and blood supply
When the inner pulp layer gets exposed or becomes irritated, this can lead to pulpitis. Later on, we’ll go through some of the reasons this might happen.
There are two main types of dental pulp inflammation: irreversible pulpitis and reversible pulpitis. Irreversible pulpitis means the infection or inflammation has gone so far that the pulp of the tooth can’t be completely saved. In contrast, reversible pulpitis can be treated and fixed if it’s caught early.
Another way that the problem can be categorized is acute pulpitis vs chronic pulpitis. The difference between acute and chronic pulpitis is that with acute pulpitis the pain comes on all of a sudden and can be quite intense, whereas chronic pulpitis is characterized by duller but longer-lasting pain.
Pulpitis symptoms and signs
Most of the time, pain is the first sign of pulpitis in a tooth. This table is a quick guide to the different symptoms you might experience, according to the type of inflammation you have:
Symptom | Reversible pulpitis | Irreversible pulpitis | Chronic pulpitis | Acute pulpitis |
General pain | Moderate | Intense, throbbing | Low, dull ache | Intense, throbbing |
Teeth sensitivity | Short and sharp | Lasts for more than 30 seconds | Short and sharp | Very painful |
Swelling around teeth | Rarely | Yes | Rarely | Yes |
Fever | Unlikely | Yes | Unlikely | Yes |
Bad breath | No | Yes | Possibly | Possibly |
Increased pain when lying down | No | Yes | No | Yes |
If you experience any of these symptoms you should visit a dentist as soon as possible. Irreversible pulpitis symptoms include extreme pain and sometimes even over-the-counter painkillers won’t help with pulpitis pain relief. If your pulpitis pain becomes unbearable you should seek an appointment with an emergency dentist.
What causes pulp inflammation and infection?
There are quite a few different ways that dental pulp can become inflamed. The most common cause is deep cavities which expose the pulp to bacteria. Tooth pulpitis occurs when the pulp is irritated or develops an infection.
Some other ways that dental pulp can become inflamed or infected include:
- Injuries or impact around the head or mouth
- A cracked, fractured, or chipped tooth that exposes the pulp layer
- Aggressive toothbrushing with abrasive toothpaste
- Grinding teeth (bruxism) causing teeth to crack or enamel and dentin to wear away
- A bad bite, or malocclusion, which can cause extra wear on certain teeth
Although uncommon, it is also possible to get tooth pulp inflammation from routine dental visits. For example:
- Pulpitis after a filling can occur due to teeth being exposed to extreme heat when setting the materials.
- The heat caused by tooth polishing may cause inflammation.
- Dental pulp can be exposed to bacteria during a filling treatment.
- Pulpitis after having a crown fitted; this process can irritate the pulp and compromise the nerve.
If you believe you have dental pulp inflammation as a result of dental treatment, you should contact your dentist for further evaluation and treatment.
Additionally, you can check out this guide provided by the American Dental Association about how to try and resolve complaints about your dentist.
Diagnosis
This kind of diagnosis is fairly straightforward for your dentist. Four types of tests can be done to determine if you have this condition and whether it is reversible or irreversible.
- X-rays can show your dentist the extent of the tooth decay and whether it might be possible to reverse the damage.
- Exposure to heat, cold, and sweet things will help your dentist know if the nerve in your tooth is still intact.
- Tooth tap tests are done to tell your dentist how inflamed your tooth is.
- Electric testing involves passing a small electrical current through the tooth. If you can feel the electricity this means your tooth is still alive and the problem is reversible.
The video below explains what pulpitis is and what the differences are between reversible and irreversible pulpitis:
Pulpitis treatment options
Since there are several different types, there are also several possible treatments. Your dentist will complete some tests to see whether your tooth can still be saved with reversible pulpitis treatment, or whether you need a tooth extracted for irreversible pulpitis treatment.
Reversible pulpitis treatment
Your tooth can be saved if you seek early treatment for reversible pulpitis. During reversible pulpitis treatment, your dentist will remove any cavities and add a filling to stop the pulp being exposed. Similarly, tooth pulpitis caused by a crack in the tooth can also be treated with a crown.
Irreversible pulpitis treatment
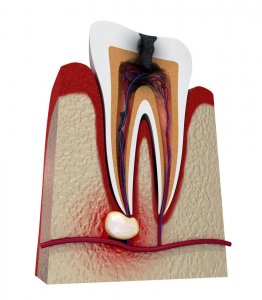
When the pulp in a tooth has died, it can’t be restored or recovered. However, it may still be possible to save the affected tooth. With a diagnosis of irreversible pulpitis, dentists can perform a root canal procedure to remove the pulp tissue. The tooth is then filled and sealed, most often with a crown, and should look and feel normal again.
Where root canal treatment isn’t viable, usually because the damage has spread too far, the only remaining treatment option is an extraction. After this, there are a number of ways to replace the missing tooth including dentures, a bridge or an implant.
If you find out that your pulpitis is irreversible, don’t panic; with a root canal, or extraction and implant, your smile will look and feel as good as new.
You’re probably also wondering about pain relief for irreversible pulpitis. The best pain relief will be getting the proper treatment from your dentist, as pain will begin to go away as soon as the pulpitis is gone. Your dentist may choose to prescribe you painkillers, but over-the-counter analgesics may help as well. In any case, be sure to ask your dentist what they advise during treatment.
Pulpitis and antibiotics
Some dentists may prescribe antibiotics to try and relieve pain and reduce inflammation in cases of irreversible pulpitis. There isn’t much evidence that antibiotics help in relieving the pain, so if you’re concerned about taking antibiotics for pulpitis, chat with your dentist.
If left untreated, it can lead to a tooth abscess, which is a pocket of infection at the base of the tooth around the gums. In this case, antibiotics are likely to be used as part of a larger course of treatment to remove the infection and treat or extract the tooth causing the problems.
Once common antibiotic, which you can read about in our guide, is amoxicillin for tooth infection.
Conclusion
There are two main types of pulpitis: reversible and irreversible. Both occur when the innermost layer of the teeth, the pulp which holds the nerves and blood supply, gets inflamed. Pulpitis pain can be intense in the case of acute pulpitis, or weaker in the case of chronic pulpitis.
Treated early, reversible pulpitis can be fixed with a simple filling. Without early intervention, the pulp can die and the problem becomes irreversible. At this point, the only options are root canal treatment or tooth extraction.
Oral health problems like this are generally avoidable with good oral hygiene and regular dentist visits. It’s not a nice problem to encounter with your teeth, so prevention is definitely better than a cure.
FAQs
How can I prevent pulpitis?

It’s pretty easy to avoid ever having to deal with it. Since the most common cause of pulp inflammation is cavities and decay, you can avoid foods with lots of sugar and acid to protect your tooth enamel. Having a good oral hygiene routine will certainly help too; brushing, flossing, and using mouthwash regularly all work towards preventing decay.
Also, be sure to have regular checkups at the dentist. A cavity spotted early can be filled before it gets anywhere near the pulp to cause painful problems.
How long does reversible pulpitis last?
If you have reversible pulpitis, you’ll want to know how long it takes to heal. Well, as soon as you have the cavity removed, your pain and inflammation should stop. It’s really important to get to a dentist as soon as possible when you get any type of toothache. Catching this problem early can mean the difference between a simple filling and a lengthy root canal treatment, or even losing the tooth entirely.
Can I get pulpitis treatment with my insurance?

If you purchased your insurance through the Affordable Care Act, or have private insurance, you need to ask your insurance provider if they will cover your pulpitis treatment. If your child is on Medicaid or CHIP, treatment should be covered by the insurance. If you are an adult on Medicaid, you’ll have to ask your state’s Medicaid program if pulpitis treatment is covered.
Read more about what is covered under Medicare, CHIP and Medicaid for dental.
What is the difference between reversible vs irreversible pulpitis?
Reversible pulpitis means that your tooth can still be saved. Your dentist will figure out where the source of the problem is—usually a cavity—and take out any decay. Irreversible pulpitis is when the pulp inside the tooth can’t be saved. You may, however, still get to keep the tooth. Your dentist might perform a root canal to remove the decayed root. If the tooth can’t be saved, then an extraction will be necessary. Irreversible pulpitis symptoms include pain, sensitive teeth, inflammation, fever, swollen lymph nodes and bad breath. Symptoms of reversible pulpitis also include pain, sensitivity and inflammation.
Will pulpitis go away?
With proper dental treatment, this condition will indeed go away. The type of treatment required may vary depending on if you have irreversible vs reversible pulpitis.
Can you treat pulpitis at home?
Unfortunately, this is a serious condition that requires professional care. You must go to the dentist for pulpitis treatment. Even if you have reversible pulpitis, your dentist will need to treat it.
If you try to treat your pulpitis at home, you may end up with a potentially lethal infection.
What is the best pulpitis pain relief?
If you need pulpitis pain relief while waiting for your dentist appointment, or after receiving pulpitis treatment, over the counter analgesics like ibuprofen and acetaminophen may help.
No pain relief treatment is to be used as a substitute for treatment from your dentist, and during your treatment, you should ask your dentist their recommendations for pain relief options.
CDA Oasis: What is the best antibiotic to prescribe for irreversible pulpitis? Consulted 24th August 2019.
MSD Manual: Pulpitis. Consulted 24th August 2019.
ADA: Problems With Your Dentist. Consulted 13 September 2019.




